This measure focuses on the four highest incidence cancers in Aboriginal and Torres Strait Islander people: prostate, breast, colorectal and lung. Data on the surgical treatment activity for these cancers at a population-level contribute to our understanding of evidence-based best-practice care.
The data presented here provide an overview of the number of cancer surgical treatments provided in Australian hospitals for patients with a principal diagnosis of cancer. Initial data for these four cancers for the years 2010 to 2015 inclusive were retrieved and analysed, and frequencies of surgical treatment by cancer principal diagnosis is presented in the following sections.
The data refer to hospital separations, not individual patients, meaning that an individual may have more than one hospital separation during the primary treatment of their cancer. A hospital separation refers to an episode of admitted patient care which can be a total hospital stay (from admission to discharge or transfer) or a portion of a hospital stay beginning or ending in a type of care (for example from acute care to rehabilitation).
For the purposes of these analyses, cancer related treatments include “key selected surgical procedures performed with the general intent to change the outcome of the cancer and/ or provide symptom relief/palliative care”.
About this measure
To determine the frequency of surgical procedures undertaken for the treatment of newly diagnosed cancers, a dataset of key selected surgical treatments has been developed for patients with a principal diagnosis of: prostate (C61), breast (C50), colorectal (C18-20), or lung (C33-34) cancer. Initial examination of procedure codes by principal diagnosis indicated a degree of overlap for treatment procedures recorded for colon and rectal cancers. To avoid potential confusion in reporting the data, these cancers have been analysed as a group (i.e. colorectal cancers).
The age-standardised incidence rates for each of these cancers for 2008-2012 are provided below:
Table 1: Incidence rates (2008-2012)
Cancer | Incidence per 100,000 persons (2008-2012) |
Prostate | 105.7 |
Breast | 94.2 |
Colorectal | 51.7 |
Lung | 81.8 |
Source: AIHW 20173
Surgical treatment for these cancers depends on the tumour size and spread, the severity of symptoms and the patient’s age and general health, as well as the use of radiotherapy and chemotherapy. Surgical treatment usually involves removing the tumour and part or all of the surrounding tissue. In certain cases, best practice guidelines also recommend the removal of one or more lymph nodes.2 For detailed information on the data including the surgical treatment procedure codes and definitions of key terms, see the NCCI ‘Surgical treatment activity – top 5 incident cancers’ page.
Current status
Key selected surgical procedures for cancer treatment (admitted patients) for Aboriginal and Torres Strait Islander people
Key selected surgical procedures for Aboriginal and Torres Strait Islander people relate to treatment for prostate, breast, colorectal, and lung cancers. The age-standardised hospital separation rate for surgical procedures for each of these cancers are provided in Table 2:
Table 2: Hospital Separations (2011-2015)
Cancer | Separations per 100,000 persons |
Prostate | 42.3 |
Breast | 94.2 |
Colorectal | 35.5 |
Lung | 11.2 |
Aboriginal and Torres Strait Islander peoples have an age structure which is notably younger than for the overall Australian population. As age is strongly related to cancer diagnoses, it is especially important that comparisons should take these differences into account. More information about the scope and data sources for surgical treatment activity data can be found in the ‘About the Data’ tab and definitions of key terms are provided in the ‘Glossary’ page. For more in-depth analysis of hospital separation rates and a comparison with the broader Australian community see the NCCI 'Surgical treatment activity for Aboriginal and Torres Strait Islander Peoples'.
Hospital separation rates compared to the rate of cancer diagnosis for Aboriginal and Torres Strait Islander people
The number and type of surgical procedures for the treatment of different cancer types and the frequency of individual cancers will vary. To allow for these differences and provide additional context for the hospital separations, the amount of hospital separations (rate of hospital separations) (Table 2) were compared with the annual rate of new cancer diagnoses (incidence) (Table 1).
This is not a direct comparison as an individual may have more than one procedure type in a given year, but it does provide an indication of whether hospital separations are relatively high or low when compared to incidence. Therefore, a ratio of close to 1 suggests that hospital separations for a particular cancer type are approximately aligned with the incidence rate for that cancer.
A comparison of the ratio of the hospital separation rates (standardised by age) and relevant incidence rates for the individual cancers (Table 3) showed that the rate of hospital separations aligned for breast cancer (ratio of 1.00) but was lower than the incidence rate for:
- Colorectal cancer (ratio of 0.69);
- Lung cancer (ratio of 0.14); and
- Prostate cancer (ratio of 0.40).
Table 3: Age-standardised separation rates (2011-2015) and age-standardised incidence ratios (2008 to 2012)
Separations per 100,000 | Incidence per 100,000 | Rate ratio | |
Prostate (C61) | 42.3 | 105.7 | 0.40 |
Breast (C50) | 94.2 | 94.2 | 1.00 |
Colorectal (C18-C20) | 35.5 | 51.7 | 0.69 |
Lung (C33-C34) | 11.2 | 81.8 | 0.14 |
Table 1, 2 and 3 notes:
- Data sourced from the National Hospital Morbidity Database (NHMD). Data on Indigenous status are considered to be of sufficient quality for analysis purposes for New South Wales, Victoria, Queensland, South Australia, Western Australia and the Northern Territory (public hospitals only).
- Separations are for patients with a principal diagnosis of specified cancer (refer to ‘About the Data' for ICD codes).
- Surgical treatment activity is for key selected procedures for the primary treatment, symptom relief or palliative care of the relevant cancer type. Refer to 'About the Data' for a full list of procedure codes, inclusion and exclusion parameters.
- Expected numbers are based on the indirect age standardisation method.
- ‘Ratio’ represents the ratio of the number observed separations for key selected procedures to the number of expected number of separations if the study population separation rate as the reference population.
- Age-standardised incidence rates sourced from AIHW: Cancer in Australia 2017. Note that these rates include cancer diagnoses by Indigenous status for all Australian jurisdictions.
- Separations are for patients with a principal diagnosis of specified cancer (refer to ‘About the Data' for ICD codes).
- ‘Rate ratio’ represents the ratio of the indirectly age-standardised separation rate (2011 to 2015) to the directly age-standardised incidence rate (2008 to 2012).
- Refer to 'About the Data' for details on methodology for calculating these estimates.
About the data
Aboriginal and Torres Strait Islander people represented around 3% of the Australian population in 2016 and have an age structure which is notably younger than for the Australian population overall.1 When examining data for Aboriginal and Torres Strait Islander people, data is presented using age standardisation ratios for Aboriginal and Torres Strait Islander peoples. The ratios are calculated by dividing the number of observed separations by the number that would have been expected from the same age-specific rates (those for the total population). These ratios are multiplied by the common crude rate for the total population to give the indirectly standardised rates.
Due to the smaller population size and therefore the numbers of procedures for Aboriginal and Torres Strait Islander people, this analysis shows indirectly age-standardised ratios for key selected surgical procedures for admitted patients with a principal diagnosis of the relevant cancer for the five-year period between 2011 and 2015. Indirectly age-standardised rates are presented for Aboriginal and Torres Strait Islander people.
This measure shows the distribution of hospital separations for key selected surgical procedures (see list below), for admitted patients with a principal diagnosis of the relevant cancer between 2011 and 2015.
Unit of analysis:
Expected separations and indirectly age standardised rates are calculated from the number of hospital separations observed where the principal diagnosis for a relevant cancer were recorded and where at least one cancer-related procedure listed below was performed. This section presents the following measures for Indigenous Australians and other Australians:
- Indirectly age standardised separations’ rates
- Ratios of indirectly age standardised separation rates to directly age standardised cancer incidence rates
In this data summary, ratios of indirectly age-standardised separations rates and directly age-standardised cancer incidence rates are presented. Directly age-standardised incidence rates were sourced from the AIHW Cancer in Australia 2017 and include cancer diagnoses from all jurisdictions. Ratios of standardised separation and incidence rates presented will therefore be a slight underestimate of the true figure as separation data from the NHMD by Indigenous status are not available for the Australian Capital Territory and Tasmania. The unavailable data for these jurisdictions is not expected to have a large effect on the separation to incidence ratios as Aboriginal and Torres Strait Islander people in Australian Capital Territory and Tasmania account for a relatively small proportion (<5% in 2016) of all Aboriginal and Torres Strait Islander people.1
For comparison, indirectly age-standardised incidence rates were calculated and there were no notable differences in the rates (and rate ratios) calculated using the direct or indirect method.
Data source:
The data for this measure are sourced from the AIHW National Hospital Morbidity Database (NHMD). The AIHW NHMD is a compilation of episode-level records from admitted patient morbidity data collection systems in Australian hospitals. The data supplied are based on the National Minimum Data Set (NMDS) for Admitted patient care; they include demographic, administrative and length of stay data, as well as data on the diagnoses of the patients, the procedures they underwent in hospital and external causes of injury and poisoning.
The scope of the NMDS is episodes of care for admitted patients in all public and private acute and psychiatric hospitals, free-standing day hospital facilities, and alcohol and drug treatment centres in Australia. Hospitals operated by the Australian Defence Force, corrections authorities and in Australia’s off-shore territories are not in scope, but some are included.2
More information about the NHMD and definitions used can be found in Appendices A and B of Admitted patient care 2015-16: Australian hospital statistics.2
Age standardised cancer incidence rates were sourced from the AIHW Cancer in Australia 2017: Chapter 8, Key population groups supplementary tables.3
Methodology for age standardisation (indirect):
Age standardisation refers to a method of adjusting for differences in age structure when comparing different populations. This is often necessary as diagnosis and separation rates are strongly related to age. There are two methods for calculating age standardised rates: direct and indirect standardisation.
For this indicator, the indirect method was used to calculate age standardised separation rates. Indirectly age standardised rates (ASR(ind)) were calculated as the weighted average of the age-specific rate ratios, where the weights are the expected number of separations on each age group of the population being compared4:
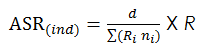
Where:
ASR(ind) = Indirect age standardised rate
d = The observed number of separations for the comparison population (Indigenous/Other Australians)
i = Age groups used for standardisation
Σ(Rini) = Expected number of separations
Ri = Age-group specific rate in age group i for the standard population
ni = Population in age group i for the comparison population(Indigenous/Other Australians)
R = Crude rate for standard population (per 100,000 persons)
Age standardised separation ratios are based on the aggregated number of separations for the 2011 to 2015, inclusive. For the purposes of this calculation, the age groups used for standardisation were: 0-39 years, 40-44 years, 45-54 years, 55-59 years, 60-64 years, 65-69, 70-74 years, 75 years and over.
Note: Direct age standardisation was not a suitable method for the present data due to the small number of hospital separations (<25) for some Indigenous Australian age groups for key selected surgical procedures with a principal diagnosis of cancer. Calculation of directly age standardised rates using the available data was not considered to be reliable for reporting purposes.4 Selection of the standard population as all Australians (instead of other Australians) was considered to be appropriate as Aboriginal and Torres Strait Islander peoples accounted for a relatively small proportion of all Australians (<3%).1
For these analyses, confidence intervals have not been included due to lack of independence between observations.
Admitted patient procedures:
Some admitted patient procedures included may have been diagnostic for a particular cancer rather than a specific treatment for the cancer. The following procedure codes defined by the Australian Classification of Health Interventions (ACHI) 6th-8th edition were included in the analysis. The ACHI is based on the Medicare Benefits Schedule (MBS) and was developed by the National Centre for Classification in Health (NCCH). For further information on the ACHI please refer to the Australian Consortium for Classification and Development website.
Cancer type | Procedure group | ACHI codes (6th-8th edition) |
Breast* | Breast excision | 31500-00 |
Breast re-excision | 31515-00 | |
Subcutaneous mastectomy | 31524-00, 31524-01 | |
Simple mastectomy | 31518-00, 31518-01 | |
Sentinel Lymph Node Biopsy (SLNB) | 30300-00, 30300-01 | |
Lymph node excision (Internal mammary/ Axilla) | 30075-11, 30332-00, 30335-00, 30336-00 | |
Colorectal | Anterior rectal resections | 32024-00, 32025-00, 32026-00, 32028-00, 92208-00 |
Hemicolectomy | 32000-03, 32000-01, 32003-01, 32003-03, 32004-01, 32005-01, 32005-03, 32006-00, 32006-01, 32006-02, 32006-03 | |
Colectomy | 32005-02, 32009-00, 32009-01, 32012-00, 32012-01 | |
Proctectomy | 32039-00, 32047-00 | |
Proctocolectomy | 32015-00, 32051-00, 32051-01 | |
Rectosigmoidectomy | 32030-00, 32030-01, 32112-00 | |
Other colorectal procedures | 30392-00, 30479-02, 32000-00, 32000-02, 32003-00, 32099-00, 90308-00, 90959-00, 30479-01, 32105-00, 32108-00, 90297-02, 90341-00 | |
Lung | Palliative procedures (pleurectomy and excision of lesion) | 38424-00**, 41892-01**, 41901-00** |
Portion of lung (segmental/wedge resections) | 38438-00, 38440-00, 38440-01, 90169-00 | |
Lobe of lung (lobectomy) | 38438-01, 38441-00 | |
Whole lung (pneumonectomy) | 38438-02, 38441-01 | |
Melanoma | Excision of lesion | 31205-00, 31230-00, 31230-01, 31230-02, 31230-03, 31230-04, 31230-05, 31235-00, 31235-01, 31235-02, 31235-03, 31235-04 |
Wedge excision | 45665-00, 45665-01, 45665-02 | |
Other melanoma/ skin procedures | 45668-00, 31000-00, 30205-00, 30205-01, 31205-01, 90403-00, 90440-00 | |
Sentinel Lymph Node Biopsy (SLNB) | 30300-00, 30300-01 | |
Prostate | Radical prostatectomies | 37210-00, 37210-01, 37211-00, 37211-01 |
Radical prostatectomies (NOS) | 37209-00***, 37209-01*** | |
Other prostate procedures | 37203-02, 37203-03, 37203-05, 37203-06, 37224-00 37224-01, 37207-00, 37207-01 | |
Brachytherapy implant | 37227-00 | |
TURP | 37203-00*** |
* For breast cancer related hospital separations, “breast reconstruction” procedures have not been included as these may not necessarily be intended for the treatment of breast cancer
** The lung cancer admitted patient procedures “pleurectomy” (38424-00) and “excision of lesion” (41892-01, 41901-00) are not intended to treat lung cancer directly and are intended for symptom relief or palliative care.
***The prostate cancer procedures “Transurethral resection of the prostate” (37203-00), “Radical prostatectomy (NOS)” (37209-00), and “Laparoscopic radical prostatectomy (NOS)” (37209-01) are procedures that may result in the diagnosis of prostate cancer and are not a specific treatment for prostate cancer.
Further information on the data excluded from the analysis is available at ‘About the data’ on the Surgical treatment activity page on the NCCI website
Data caveats:
- NHMD data on Indigenous status are considered to be of sufficient quality for analysis purposes for New South Wales, Victoria, Queensland, South Australia, Western Australia and the Northern Territory (public hospitals only).
- “Other Australians” includes separations for which Indigenous status was not reported.
- Data for “Laparoscopic right hemicolectomy with anastomosis” procedures (ACHI code 32003-03) with a principal diagnosis of colorectal cancer (C18-C20) were unavailable by Indigenous status. To allow for comparisons between these groups to the standard population (all Australians), these procedures have also been excluded from the number separations for the standard population.
- Expected number of separations and separation rates were obtained by applying standard age-specific rates for the reference population to the age-distributions of the relevant groups being studied (Indigenous and other Australians).
- Directly age standardised incidence rates were sourced from the AIHW Cancer in Australia 2017 and include cancer diagnoses from all jurisdictions. Rate ratios will therefore be an underestimate of the true figure as separation data from the NHMD by Indigenous status are not available for the Australian Capital Territory and Tasmania.
References
Activity in this area
Cancer Australia. National Aboriginal and Torres Strait Islander Cancer Framework. 2015 Available from: https://canceraustralia.gov.au/publications-and-resources/cancer-australia-publications/overlay-context=affected-cancer/aboriginal-and-torres-strait-islander-people/national-aboriginal-and-torres-strait-islander-cancer-framework
Cancer Australia. Optimal Care Pathway for Aboriginal and Torres Strait Islander people with cancer. 2018 Available from: https://canceraustralia.gov.au/publications-and-resources/cancer-australia-publications/optimal-care-pathway-aboriginal-and-torres-strait-islander-people-cancer
Data - General
Australian Institute of Health and Welfare 2017. Admitted patient care 2015–16: Australian hospital statistics. Health services series no. 75. Cat. no. HSE 185. Canberra: AIHW.
Medicare Benefits Schedule (MBS) - Items by Patient Demographics Report. Available from: http://www.data.gov.au/dataset/medicare-benefits-schedule-mbs-group-by-patient-demographics-report
Breast cancer
Cancer Australia – Breast Cancer. Available from: https://canceraustralia.gov.au/affected-cancer/cancer-types/breast-cancer (accessed January 2017).
Australian Institute of Health and Welfare 2015. Breast cancer in young women: key facts about breast cancer in women in their 20s and 30s. Cancer series no. 96. Cat. No. CAN 94. Canberra: AIHW.
Lung cancer
Cancer Australia – Lung Cancer. Available from https://lung-cancer.canceraustralia.gov.au/ (accessed May 2017).
Cancer Australia. Report to the Nation - Lung Cancer 2011. Cancer Australia, Sydney, NSW, 2011.
Prostate cancer
Cancer Australia – Prostate Cancer. Available from https://prostate-cancer.canceraustralia.gov.au (accessed May 2017).
Colorectal cancer
Cancer Australia – Bowel Cancer. Available from https://bowel-cancer.canceraustralia.gov.au/ (accessed May 2017).
References
1. Australian Bureau of Statistics 2017. Census of Population and Housing: Reflecting Australia - Stories from the Census, 2016. ABS cat. no. 2071.0. Canberra: ABS.
2. Australian Institute of Health and Welfare 2017. Admitted patient care 2015–16: Australian hospital statistics. Health services series no. 75. Cat. no. HSE 185. Canberra: AIHW.
3. Australian Institute of Health and Welfare 2017. Cancer in Australia 2017. Cancer series no.101. Cat. no. CAN 100. Canberra: AIHW.
4. Australian Institute of Health and Welfare 2011. Principles on the use of direct age-standardisation in administrative data collections: for measuring the gap between Indigenous and non-Indigenous Australians. Cat. no. CSI 12. Canberra: AIHW.